Have you heard of B-lines?
B-lines are a common finding on lung ultrasonography in all species. If you are not familiar with the term, you may know them by another name: “comet tails,” “sprays” or “rockets.”
What exactly are they?
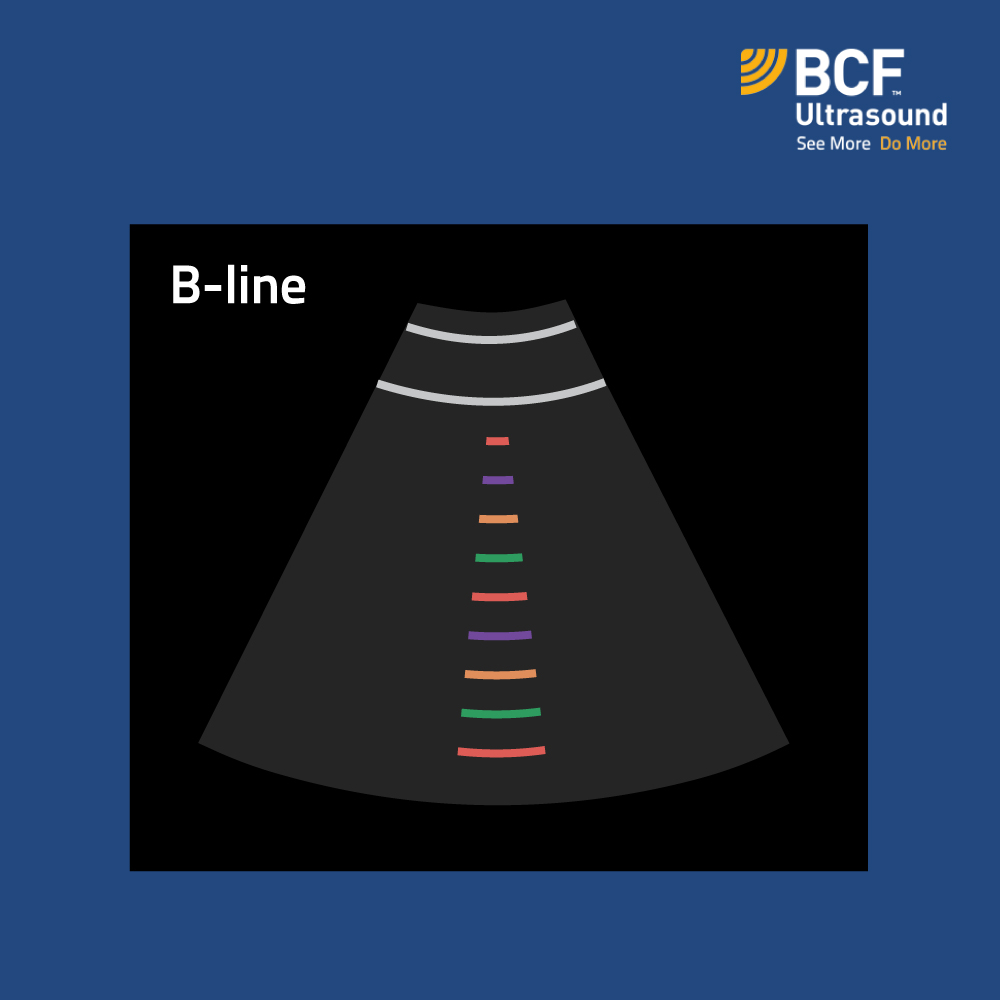
There are 7 key criteria that we can apply to B-lines (Lichtenstein D., 2013):
- “Comet-tail” appearance and VERTICAL orientation (in contrast to HORIZONTAL A-lines).
- Arise from the pleural line.
- Move with lung sliding.
- Do not fade (i.e., they “shoot” down to the bottom of the screen). This characteristic depends on the width of the base – see clip below.
- Well-defined.
- Hyperechoic.
- Obliterate the appearance of A-lines.
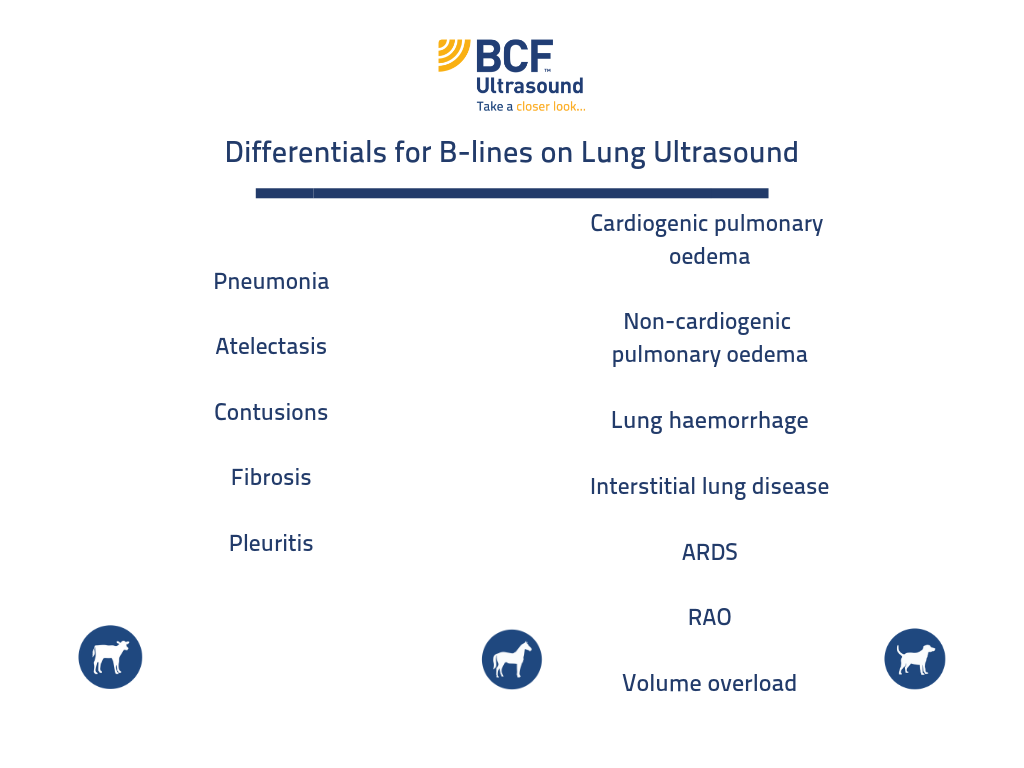
Isolated B-lines or the presence of a few narrow-based “comet tails” are not uncommon findings in healthy patients.
Meanwhile, broad-based B-lines or numerous narrow-based “comet tails” are more significant. BUT you should always interpret the significance based on history and concurrent clinical findings.
In this clip, you can see the difference between narrow-based comet tails in a healthy horse’s chest, vs. the appearance of wide-base comet tails in a cat in respiratory distress.
https://www.high-endrolex.com/19
In which conditions will we see B-lines on our chest scan?
Key Points About B-Lines:
- They are a lung-surface phenomenon. If you are concerned about issues deep in the lung parenchyma, other diagnostics still need to be utilized (e.g., radiography, CT). Remember the case example of the foal from Part 1. In that case, the lung surface was within normal limits, but mediastinal abscesses were present.
- They precede the development of alveolar flooding and subsequent consolidation. If B-lines are the only abnormality you identify on lung ultrasound, this could be good news for you! If you recognize changes early on and instigate appropriate treatment quickly, you have a better chance of getting on top of the lung disease – improving the patients’ diagnosis.
References:
Lichtenstein D. FALLS-protocol: Lung ultrasound in hemodynamic assessment of shock. Heart, Lung, and Vessels. 2013; 5(3): 142-147.